Autoimmune Pancreatitis Treatment in Kolkata
Home > Pancreatic Diseases > Autoimmune Pancreatitis
Overview
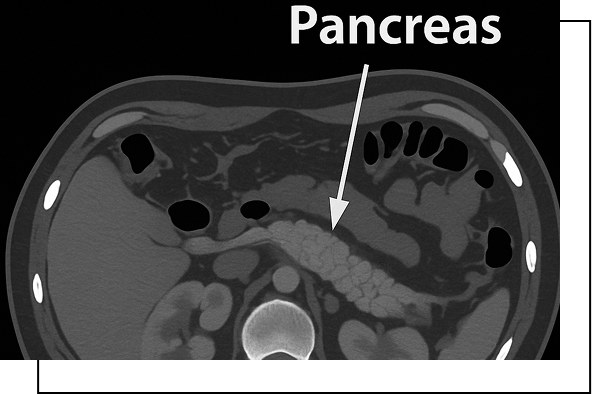
Autoimmune pancreatitis is a rare inflammatory disease of the pancreas, a gland behind your stomach that produces digestive enzymes and insulin. In this condition, the body’s immune system mistakenly attacks the healthy tissues of the pancreas, causing inflammation and potential damage. It often mimics conditions like pancreatic cancer but is treatable.
Types of Autoimmune Pancreatitis
There are two primary types of autoimmune pancreatitis:
Type 1 Autoimmune Pancreatitis (IgG4-related sclerosing pancreatitis)
Characterized by the presence of a protein called IgG4 in the inflamed tissue, generally common in older individuals and linked to other autoimmune diseases such as sclerosing cholangitis.
Type 2 Autoimmune Pancreatitis (Lymphocyte Epithelial Destruction associated with Sclerosing Sialadenitis)
Associated with inflammation of the salivary glands and the pancreas, more common in younger people.
Autoimmune Pancreatitis Symptoms
Consult an autoimmune pancreatitis doctor in Kolkata immediately if any or multiple of these symptoms persist. Patients may experience the following autoimmune pancreatitis symptoms:
Persistent abdominal pain
Poor appetite and sudden weight loss
Jaundice (yellowing of the skin or eyes)
Diabetes onset or worsening
Fatigue
Dark urine
Fatigue
Dark urine
Causes and Risk Factors
The proper cause is unclear, but autoimmune pancreatitis is associated with immune system malfunctions. Factors include:
Genetic predisposition
Environmental triggers and smoking history
More common in men over 50
Other autoimmune disorders
Book An Appointment
Evaluation
Visit a doctor for acute pancreatitis treatment in Kolkata for an expert diagnosis and tailored treatment plan.
Blood tests for IgG4 levels
Imaging tests like CT scan or MRIs
Biopsy
Corticosteroid trial
Here are some autoimmune pancreatitis diagnostic criteria:
Pancreatic Imaging
Imaging studies typically show diffuse pancreatic enlargement with irregular narrowing of the primary pancreatic duct, often involving a significant portion of the gland.
Laboratory Findings
Common findings include elevated serum gamma globulin or IgG levels and the presence of autoantibodies.
Histopathology
Biopsy samples often reveal fibrotic tissue changes with prominent infiltration by lymphocytes and plasma cells.

Management
Autoimmune pancreatitis treatment focuses on three key areas:
Corticosteroids
Steroid medications
Immunosuppressant drugs
Long-term Monitoring
An autoimmune pancreatitis diet focusing on low-fat, nutrient-rich foods
Follow-up care is essential
Maintain a healthy lifestyle
Limit of smoking
Book An Appointment
FAQs
Know Your Answers
Can autoimmune pancreatitis imitate cancer?
Yes, it can imitate pancreatic cancer. Your doctor will prescribe imaging and biopsies to differentiate and provide proper treatments.
How is it different from regular pancreatitis?
AIP responds well to steroids, unlike other forms of pancreatitis caused by alcohol or gallstones.
What foods to avoid with AIP?
Avoid high-fat, sugary, and processed foods. Consult a dietitian for personalized advice.
Is autoimmune pancreatitis life-threatening?
With timely treatment, most cases are manageable and non-fatal.
What's the success rate of treatment?
Most patients (80%) respond well to initial steroid therapy with proper medical guidance.

